When you feel stuck in a mental loop, wonder why everyday tasks seem heavy, or notice a persistent sense of unease, you’re likely facing psychological problems. Solving them isn’t a magic trick; it’s a step‑by‑step process that blends self‑awareness, proven therapeutic tools, and sometimes professional help.
Identify What You’re Dealing With
Psychological problems are mental‑health issues that affect thoughts, emotions, or behavior, ranging from mild stress to severe mood disorders. Before you can address them, you need a clear picture of the symptoms:
- Persistent sadness or irritability
- Excessive worry or panic attacks
- Obsessive thoughts or compulsive actions
- Difficulty sleeping, eating, or concentrating
- Physical tension that doesn’t go away
Jot these down in a journal for a week. Patterns will emerge, and you’ll have concrete evidence to discuss with a professional if needed.
Choose the Right Approach
There isn’t a one‑size‑fits‑all solution. Think of treatment options as a toolbox; you pick the tool that matches the job.
- Cognitive Behavioral Therapy (CBT) - focuses on changing distorted thoughts and unhelpful behaviors.
- Mindfulness‑Based Stress Reduction (MBSR) - teaches you to stay present and observe thoughts without judgment.
- Dialectical Behavior Therapy (DBT) - combines CBT with skills for emotional regulation and interpersonal effectiveness.
- Medication - antidepressants, anxiolytics, or mood stabilizers prescribed by a psychiatrist.
- Support groups - peer‑led meetings that provide shared experience and accountability.
Most people benefit from a blend: therapy for skill‑building, medication for biochemical balance, and self‑help tactics for day‑to‑day resilience.
Start With Self‑Help Strategies
Even before you book an appointment, these habits can lower the intensity of many psychological problems.
- Schedule regular movement. A 30‑minute walk releases endorphins and improves mood.
- Practice nightly gratitude. Write three things you appreciated that day to rewire negative thought loops.
- Limit caffeine and alcohol. Both can amplify anxiety and disrupt sleep.
- Set boundaries on social media. Reduce exposure to comparison triggers that fuel low self‑esteem.
- Use a simple breathing exercise. Inhale for 4 seconds, hold for 4, exhale for 6 - repeat five times.
These actions create a stable foundation that makes therapy more effective.
When and How to Seek Professional Help
Self‑help works for many mild issues, but if any of the following apply, it’s time to consult a specialist:
- Thoughts of self‑harm or suicide
- Symptoms lasting more than two months without improvement
- Interference with work, school, or relationships
- Physical symptoms (e.g., chronic headaches) that have no medical cause
Here’s a quick road‑map:
- Contact a psychiatrist for an assessment if you suspect medication might help.
- Book a session with a licensed therapist or counselor to explore talk‑based interventions.
- Ask about a trial period of CBT or DBT; many clinics offer a 6‑session intro package.
- Consider joining a local support group for shared experiences.
Be honest about your symptoms, lifestyle, and any previous attempts at self‑help. The more data you provide, the sharper the treatment plan.

Comparing Common Therapy Options
| Approach | Typical Duration | Best For | Key Technique |
|---|---|---|---|
| Cognitive Behavioral Therapy (CBT) | 12‑20 weeks | Anxiety, mild‑moderate depression | Thought‑recording, behavioral experiments |
| Dialectical Behavior Therapy (DBT) | 6‑12 months (skills groups) | Borderline personality, emotion dysregulation | Mindfulness, distress‑tolerance drills |
| Mindfulness‑Based Stress Reduction (MBSR) | 8‑week courses | Chronic stress, pain, trauma | Meditation, body‑scan |
| Medication (e.g., SSRIs) | Varies; often months to assess | Severe depression, OCD, PTSD | Neurochemical regulation |
Pick the row that matches your symptom profile and lifestyle. Many clinicians combine CBT with medication for faster relief.
Common Pitfalls and How to Avoid Them
Even with a solid plan, people trip up. Recognize these traps early:
- Expecting instant results. Therapy typically shows measurable change after 4‑6 weeks.
- Skipping homework. CBT worksheets are not optional; they reinforce session work.
- Self‑diagnosing. Relying on internet forums can mislead; a professional assessment is essential.
- Sticking to one method. If CBT isn’t clicking after a reasonable trial, discuss alternatives with your therapist.
- Ignoring physical health. Sleep, nutrition, and exercise heavily influence mental well‑being.
Keep a progress log and review it monthly. Adjust the plan based on what’s actually helping.
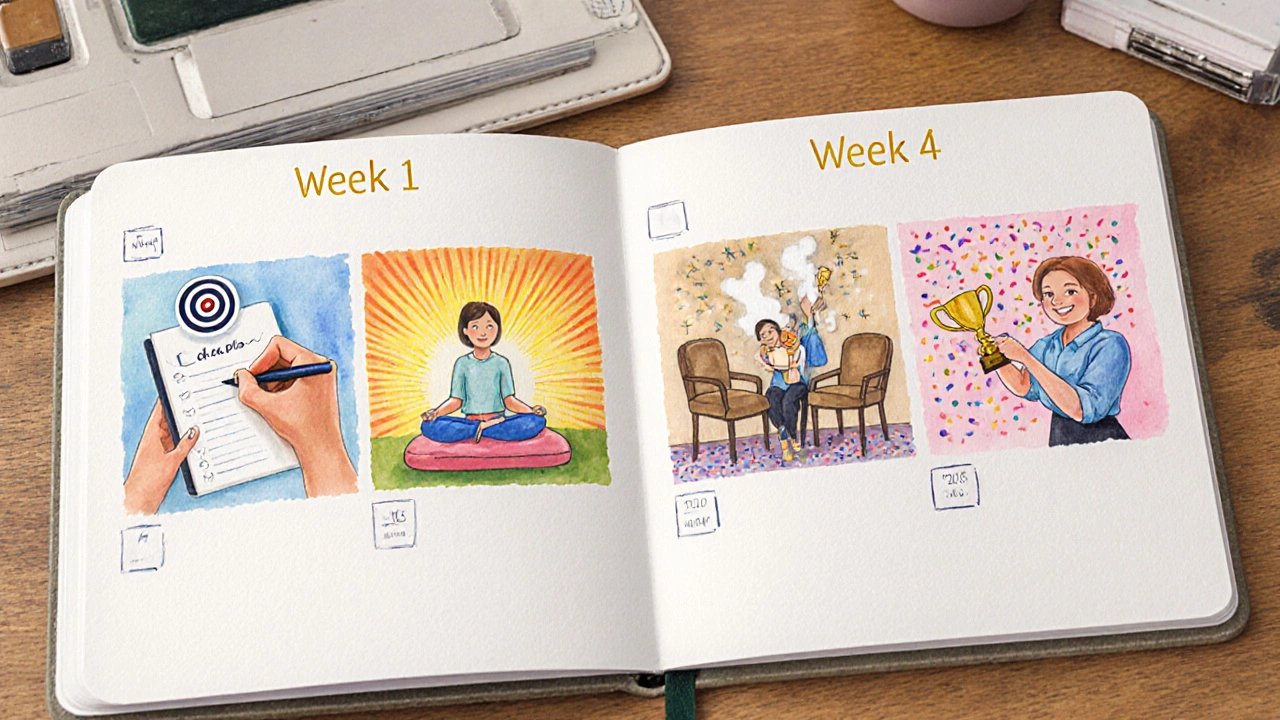
Putting It All Together - A 4‑Week Starter Plan
Use this template as a launchpad. Feel free to stretch or compress each week based on your schedule.
- Week 1 - Assessment & Goal Setting
- Complete a symptom journal (5‑10 min daily).
- Schedule a 30‑minute consult with a therapist.
- Identify 2‑3 concrete goals (e.g., “reduce panic episodes to < 2 per week”).
- Week 2 - Skill Introduction
- Learn the CBT thought‑record template and fill it each night.
- Start a daily 5‑minute mindfulness meditation.
- Add 20 minutes of moderate exercise 3 times this week.
- Week 3 - Practice & Feedback
- Bring your thought‑records to the therapist session; discuss patterns.
- Try a brief exposure exercise for a feared situation (under therapist guidance).
- Attend a local support group meeting (online or in‑person).
- Week 4 - Review & Adjust
- Rate symptom intensity on a 0‑10 scale; compare to Week 1.
- Decide whether to continue CBT, add medication, or switch to DBT skills.
- Celebrate any improvement, no matter how small.
Consistency beats intensity. Stick with the plan for at least six weeks before judging its effectiveness.
Frequently Asked Questions
Frequently Asked Questions
Can I treat anxiety without seeing a therapist?
Self‑help tools like breathing exercises, regular exercise, and mindfulness can lower mild anxiety, but if symptoms persist for more than a couple of months or interfere with daily life, professional guidance is recommended.
How long does it take for antidepressants to work?
Most SSRIs show noticeable improvement after 4‑6 weeks, though some patients feel a change sooner. It’s essential to stay in touch with the prescribing psychiatrist during this period.
Is CBT effective for depression?
Yes. Numerous studies report that CBT reduces depressive symptoms by 50‑60% when delivered weekly for 12‑20 sessions, especially when combined with medication for moderate‑to‑severe cases.
What should I expect in my first therapy session?
The therapist will ask about your current concerns, medical history, and goals. They might give you a short questionnaire and suggest a treatment approach. It’s a chance for you to see if you feel comfortable with their style.
Can support groups replace individual therapy?
Support groups provide community and shared coping tips, but they don’t offer personalized treatment plans. They’re best used alongside, not instead of, professional therapy.
Next Steps
1. Write down the symptoms you notice each day.
2. Choose one self‑help habit from the list and start today.
3. Book a 30‑minute intake with a therapist or psychiatrist within the next two weeks.
4. Use the 4‑week starter plan as a framework and adjust as you learn what works for you.
Remember, solving psychological problems is a journey, not a sprint. Small, consistent actions build the momentum needed for lasting change.