Schizophrenia Early Warning Signs Assessment
Early Warning Signs Assessment
This tool helps identify potential early warning signs of schizophrenia based on the three key indicators discussed in the article. It is not a diagnostic tool but can guide when to seek professional help. All responses are confidential.
1. Social withdrawal and loss of interest
2. Unusual thoughts or perceptual changes
3. Cognitive decline and functional impairment
Assessment Result
Important note: This assessment is for informational purposes only and should not be considered a medical diagnosis. It's designed to help identify potential warning signs and guide when professional help might be beneficial. Always consult a qualified mental health professional for proper evaluation.
Spotting the first clues of schizophrenia warning signs can feel like trying to read a book half‑written in a foreign language. The truth is, the brain often drops hints long before a formal diagnosis appears, and recognizing those hints can change the whole story for a person and their loved ones.
What is schizophrenia?
Schizophrenia is a chronic mental health condition that affects how a person thinks, feels, and behaves. It typically emerges in late adolescence or early adulthood and is characterized by a mix of positive symptoms (like hallucinations and delusions), negative symptoms (such as social withdrawal), and cognitive difficulties. The World Health Organization estimates that about 20 million people worldwide live with schizophrenia, making early awareness a public‑health priority.
Why early warning signs matter
When the first signs appear, they’re often subtle and easy to dismiss as stress, sleeplessness, or a rough teenage phase. Yet research from the National Institute of Mental Health shows that intervening during the prodromal (early) phase can reduce the severity of later episodes by up to 40 %. Early detection opens the door to therapy, medication, and lifestyle changes that can preserve education, work, and relationships.
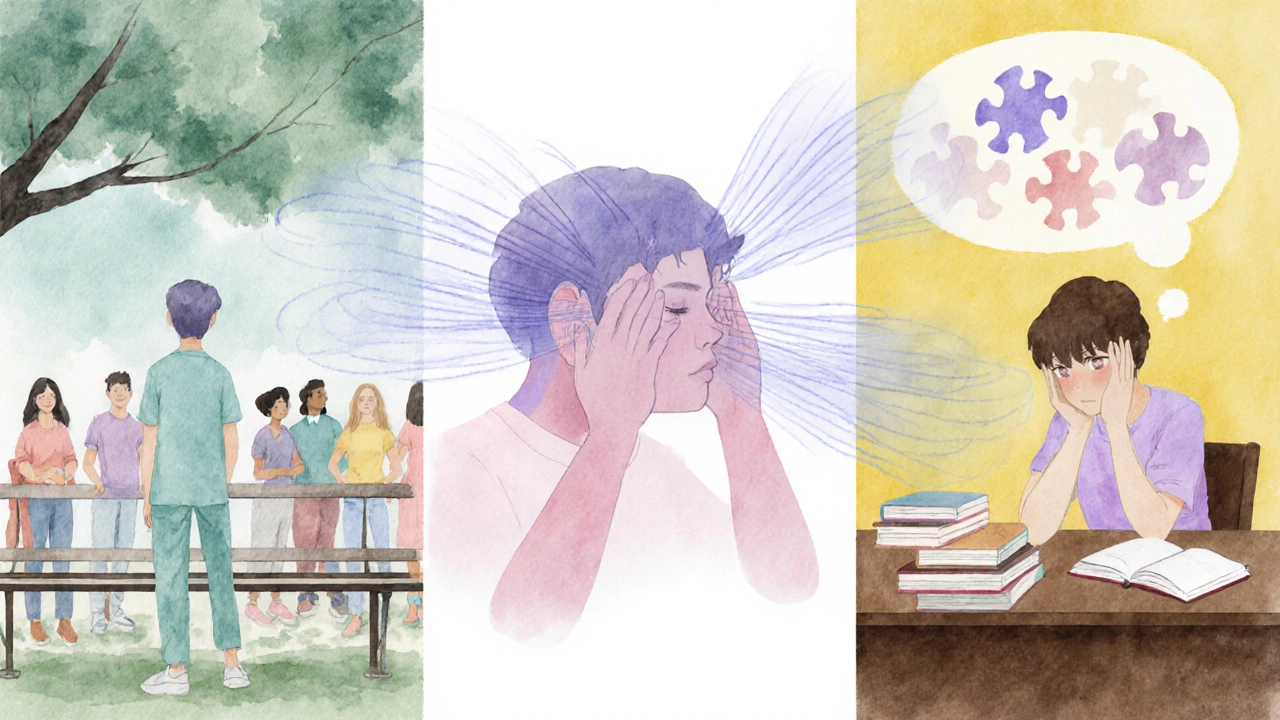
The three key warning signs
- Social withdrawal and loss of interest in activities - A once‑social person may start avoiding friends, canceling plans, and spending most of their time alone. This isn’t just shyness; it’s a negative symptom that signals the brain’s reward system is dimming. According to a 2023 longitudinal study, 60 % of individuals later diagnosed with schizophrenia reported a noticeable drop in social engagement at least six months before other symptoms emerged.
- Unusual thoughts, perceptual changes, or mild hallucinations - The mind may begin to blur the line between reality and imagination. This could look like hearing faint whispers, believing that ordinary objects have secret meanings, or feeling that thoughts are being inserted or removed. Hallucinations are sensory experiences without an external source, while delusions are fixed false beliefs. Even when these experiences are brief or mild, they are a red flag when they start to disrupt daily life.
- Cognitive decline and functional impairment - Simple tasks become harder. Someone might struggle to concentrate on a conversation, forget to take medication, or neglect personal hygiene. This cognitive slump is often the first measurable change clinicians track. A 2022 meta‑analysis found that 45 % of people in the prodromal stage showed a drop in working memory and executive function before full‑blown psychosis.
How to tell the difference from normal mood swings
Everyone feels odd thoughts or occasional loneliness, but three patterns help separate everyday stress from early schizophrenia:
- Duration - Symptoms persisting for more than a month without a clear trigger are concerning.
- Impact - If the behavior interferes with school, work, or self‑care, it’s a warning sign.
- Progression - Noticeable worsening over weeks signals a prodromal trajectory.
What to do if you notice these signs
Taking action doesn’t mean jumping straight to medication; it means gathering information and seeking professional guidance.
- Document observations - Keep a simple log of behaviors, dates, and any quotes that seem odd. This makes the next appointment more productive.
- Start a gentle conversation - Use “I’ve noticed…” statements instead of accusations. For example, “I’ve seen you’ve been staying in your room a lot lately, and I’m worried you might be feeling overwhelmed.”
- Encourage a mental‑health evaluation - Suggest seeing a psychiatrist or a qualified therapist who specializes in early psychosis. Many clinics have dedicated early‑intervention programs.
When professional help arrives
During the first assessment, clinicians will explore the three warning signs, run a brief mental‑status exam, and may use tools like the Structured Interview for Prodromal Syndromes (SIPS). If a prodromal diagnosis is made, treatment options typically include:
- Antipsychotic medication - Low‑dose atypical antipsychotics can reduce symptom intensity without heavy side effects.
- Cognitive‑behavioral therapy (CBT) - Tailored CBT addresses distorted thoughts and improves coping skills.
- Family psychoeducation - Teaching relatives about the illness cuts relapse rates by up to 30 %.

Why early intervention works
Studies from the Early Psychosis Intervention Network (EPIN) show that individuals who receive treatment within the first six months of prodromal symptoms have a 25 % higher chance of maintaining employment or education after two years. Moreover, early care reduces hospital admissions, lessening both personal and societal costs.
Quick reference table
| Sign | Typical age of appearance | Observed in prodromal stage (%) |
|---|---|---|
| Social withdrawal | 15‑22 | 60 |
| Unusual thoughts / mild hallucinations | 16‑24 | 45 |
| Cognitive decline (memory, attention) | 14‑20 | 40 |
Frequently Asked Questions
Can teenagers experience these warning signs?
Yes. Schizophrenia often begins in late teens or early twenties. While many teenagers go through mood swings, persistent social withdrawal, strange thoughts, or cognitive lapses that interfere with school warrant a professional check‑up.
Do all people with schizophrenia show all three signs?
No. The presentation varies. Some may first notice hallucinations, others might primarily experience negative symptoms like withdrawal. Recognizing any one of the key signs should still prompt further evaluation.
Is medication always required?
Not always. For many in the prodromal phase, low‑dose antipsychotics combined with psychotherapy and lifestyle changes are enough to delay or prevent full‑blown psychosis. The treatment plan is personalized.
How long does it take to get a diagnosis?
A thorough assessment usually takes one to three appointments, each lasting 60‑90 minutes. Clinicians will also gather collateral information from family or teachers.
What should I do if I suspect a loved one is showing these signs?
Start a supportive conversation, keep a simple observation log, and encourage them to see a mental‑health professional. Offer to attend the first appointment if they’re comfortable.
